This article was produced in partnership with the Mayo Clinic’s Center for Individualized Medicine. It was also published in The Huffington Post and The Mayo Clinic’s Individualized Medicine blog.
At age 42, Holly Boehle was diagnosed with aggressive breast cancer. Fortunately, the cancer cells have been banished by chemotherapy targeted against a specific genetic abnormality in her tumor. She’s now back home in Michigan with her children, husband, and friends, and has returned to her job as a school psychologist. But a record of the cancer that affected Boehle lives on in our lab at the Mayo Clinic, in a set of mice that each host a living genetic replica of her tumor and in a file that contains the tumor’s complete genetic blueprint. We can use this information to design targeted treatments for Boehle, if her cancer should ever return, and to help other women with genetically similar tumors.
Boehle is an early example of how advances in genomics are transforming cancer treatment from a one-size-fits-all model to a process tailored to the individual patient and her tumor, an approach known as personalized oncology.(a) “I think it’s pretty amazing to have mice with my tumor tissue growing inside them,” said Boehle, who was diagnosed with aggressive breast cancer in her early 40s. “This gives researchers… the opportunity to see specifically how my cancer responds to a variety of treatments.” It can also help us understand why standard chemotherapy is successful for some women, like Boehle, but not for others.
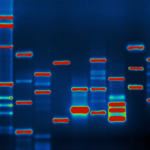
This revolution in breast cancer research and treatment is being driven by rapid advances in the field of genomics. Every cancerous tumor has a unique genetic profile that determines not only how the tumor grows, but also how it responds to chemotherapy. A precipitous drop in the cost of DNA sequencing has made it possible, for the first time, to analyze the genome of individual cancer patients and their tumors. Given the wide genomic variation that exists between one cancerous tumor and the next – and even within a single tumor – this type of individual genomic analysis is essential to understanding each patient and their cancer.
Just as importantly, by comparing massive amounts of genomic data from large numbers of patients, scientists are making new discoveries about what drives breast cancer and how it can best be treated. Researchers have identified numerous different breast-cancer-related genetic mutations, from the well-known BRCA to more obscure genes like ATM, MLH3, and NBN.(b) They are now working to identify which chemotherapy drugs work best for people with particular mutations. For example, research is underway to test the hypothesis that a group of drugs called PARP inhibitors are particularly effective in treating patients with BRCA mutations, potentially giving these patients a better chance of survival.
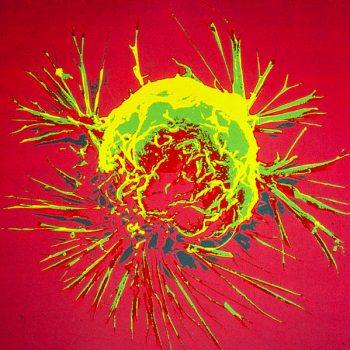
Our study, the Breast Cancer Genome Guided Therapy (BEAUTY) project, aims to advance scientific understanding of the genomics of breast cancer and, in particular, to understand these genomic alterations in the context of standard chemotherapy.1 From 2012 through 2014, 140 women with invasive breast cancer, including Boehle, enrolled in the BEAUTY study, which involved having their blood genetically sequenced and their tumors sequenced before, during, and after chemotherapy. The patients received neoadjuvant chemotherapy to shrink the tumors, we tracked the size of their tumors over time to measure how well they were responding to treatment, and then they received surgery to remove any remaining cancer. We also injected cells from their tumors into mice in a process known as xenografting.(c) For those tumors that grew in mice, these mouse “avatars” now hold a living record of the patients’ cancer, which allows us to test their tumors’ responsiveness to various drugs.2
Using the rich data we have collected on the genomic profiles of patients and their tumors, as well as their treatment outcomes, we are tracking which mutations and biomarkers predict how patients respond to standard chemotherapy. We’re also analyzing how different genetic signatures are associated with the success of specific chemotherapy drugs, so we can match patients to the most effective drugs. For instance, we’ve identified a common alteration that may affect how tumors respond to taxane, a widely-used chemotherapy drug that targets microtubules in cells. Additionally, we have identified many different cancer-related mutations in participants’ blood which may not only be associated with the initial risk of these patients developing cancer, but also with their response to chemotherapy.
One key goal of the BEAUTY study is to improve treatment options for high-risk patients whose cancer is not responsive to traditional chemotherapy.3 Using genomic data about these patients and their tumors, we can identify potentially relevant mutations. In cases where effective treatments for their specific genetic signature are unknown, we can test options on their mouse avatars.(d) This individually tailored approach is being used with BEAUTY study participants whose cancer has recurred. Participants who we’ve identified as having BRCA1 mutations, for example, may be treated with platinum-based therapy or PARP inhibitors, while other patients will receive different drugs.
This is an exciting time in breast cancer treatment and research, as we move beyond the one-size-fits-all model of the past to a personalized approach tailored to each patient. We’ll be tracking our BEAUTY patients over the next five years to learn more about how their genomic profiles predict their long-term outcomes. We’ll also be helping devise customized treatment plans if their cancers return. And while the BEAUTY study may not help each individual woman who participates today, their involvement is helping us make discoveries that will transform the lives of future patients. The hope is that one day, every woman facing cancer will receive personalized treatment that gives her the best chance of survival.
Endnotes
- Matthew P. Goetz, et al. (2013) “Integration of next generation sequencing (NGS) and patient derived xenografts (PDX) to identify novel markers of paclitaxel (T) response in the breast cancer genome guided therapy study (BEAUTY),” in Proceedings of the 36th Annual CTRC-AACR San Antonio Breast Cancer Symposium, San Antonio, TX: December 10-14, published in Cancer Research, 73: Abstract P1-08-10.
- Jia Yu, et al. (2014) “Feasibility of using percutaneous tumor biopsies from a prospective neoadjuvant breast cancer study to develop patient derived xenografts and assess in vivochemotherapy sensitivity [abstract],” in Proceedings of the 105th Annual Meeting of the American Association for Cancer Research, San Diego, CA: April 5-9, published in Cancer Research, 74: Abstract 1195.
- Krishna R. Kalari, et al. (2014) “Analysis of sequencing data to identify potential drug targets for an individual newly diagnosed with basal breast cancer who failed to respond to current standard neoadjuvant chemotherapy [abstract],” in Proceedings of the 105th Annual Meeting of the American Association for Cancer Research, San Diego, CA: April 5-9, published in Cancer Research, 74: Abstract 4185.
Sidenotes
- (a) Personalized oncology is one branch of a new field known as individualized, personalized, or precision medicine. Using genomic information, doctors can target treatment to the characteristics and needs of individual patients.
- (b) The BRCA1 and BRCA2 genes produce proteins that suppress tumors by repairing damaged DNA in cells. Hereditary mutations in these genes significantly increase the risk of breast and ovarian cancer, and account for 5 to 10% of breast cancers. Many women with a strong family history of breast cancer are now tested for BRCA mutations and, if positive, may take proactive steps to lower their risk.
- (c) Xenotransplantation is the moving of cells or tissues (xenografts) from an organism of one species to another species. It is an increasingly popular method for studying human cancer by grafting tumor cells onto mice whose immune systems are compromised so their bodies will not reject foreign tissue. Xenotransplantation can also be done in reverse, allowing animals such as pigs to serve as donors for humans in need of organs.
- (d) This type of personalized treatment is sometimes referred to as n-of-one research. N is the variable typically used to denote the sample size in a clinical trial. A study with an n of one focuses on experimentally evaluating treatment options for just one patient.